Introduction+
Vacuum assisted excision (VAE)
Vacuum assisted biopsy (VAB) was first introduced in 1995 by Fred Burbank and Mark Retchard to overcome the challenges with FNA (fine needle aspiration) and core biopsy. Despite being introduced in the mid-1990s, it took about 10-15 years for wider adoption within the breast imaging community. The concept of vacuum assisted excision stemmed from VAB.
The difference between VAB and VAE is that VAB is where the biopsy is being performed to establish a diagnosis while VAE is where a diagnosis has been made and the decision is to perform a further biopsy to either sample a larger area (aiming for about 4 grams) or to excise the lesion.
The Marmot review1 played an important role in the adoption of VAE for the management of high risk/B3 lesions and supporting trials such as the SMALL Trial2. The Marmot review1 concluded that breast screening saves lives and that for every 10 000 UK women invited to screening from age 50 for 20 years, about 681 cancers will be found, of which 129 will represent over-diagnosis, and 43 deaths from breast cancer will be prevented.
Over-diagnosis was defined1 as a cancer–invasive or non-invasive–diagnosed by screening that would not have presented during a woman’s lifetime. The focus was initially over-diagnosis but quickly this was recognised as being inevitable and the focus quickly shifted to minimising overtreatment. Following the Marmot review, a group was set up to look at minimising treatment of high risk/B3 lesions in the UK breast screening programme. This was a multi-disciplinary group consisting of radiologists, pathologists, and surgeons. The NHS Breast Screening multidisciplinary working group guidelines for the diagnosis and management of breast lesions of uncertain malignant potential on core biopsy (B3 lesions) were endorsed and adopted by the NHS Breast Screening programme in 20163 and the guidelines were published in 20184. Subsequently data was published on the impact in 20225, showing that VAE was a safe alternative to surgery for this group.
Continuing with the theme of minimising overtreatment, this was then extended at looking at good prognostic tumours (grade 1, ER positive and HER2 negative). The SMALL Trial6: Open surgery versus minimally invasive vacuum-assisted excision for small screen-detected breast cancer–a UK phase III randomised multi-centre trial was set up. This trial is looking to see if small (≤15 mm), grade 1, ER and PR positive and HER2 negative cancers can be treated with VAE rather than surgery.
The future is exciting as clinicians are using existing tools such as VAB/VAE, which are widely available, and repurposing then to help improve the patient pathway and minimise overtreatment.
The term VAE can be categorised as a diagnostic VAE or therapeutic VAE. Diagnostic vacuum assisted excision3,4,5,7 or extended vacuum assisted biopsy (DVAE or EVAB) is defined as taking a large volume of tissue (equating to about 4 grams) for further sampling of an area, accepting that if a lesion is small (≤15 mm), it may be excised in its entirety. The main aim is representative sampling of the area that would equate to a surgical diagnostic biopsy.
Therapeutic vacuum assisted excision (TVAE) is defined as using vacuum biopsy to excise a cancer–the aim would be to excise the lesion. The lesion would be excised piecemeal and therefore margins cannot be assessed with TVAE histologically. Complete excision will need to be determined by the operator performing the TVAE and post-excision imaging.
Medical VAE Indications
- Excision of benign lesions such as fibroadenomas8,9
- Management of high-risk lesions/B3 lesions3,4,5,7,10
- Excision of good prognostic tumours2,6 in the context of a trial
VAE Procedure
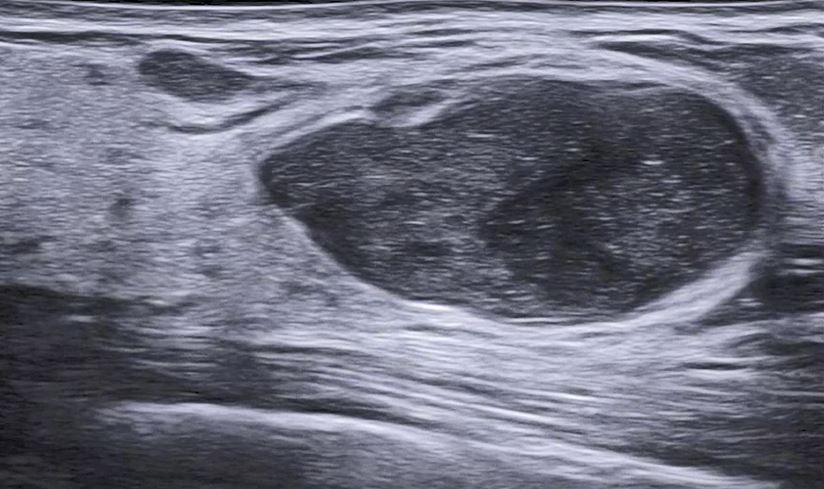
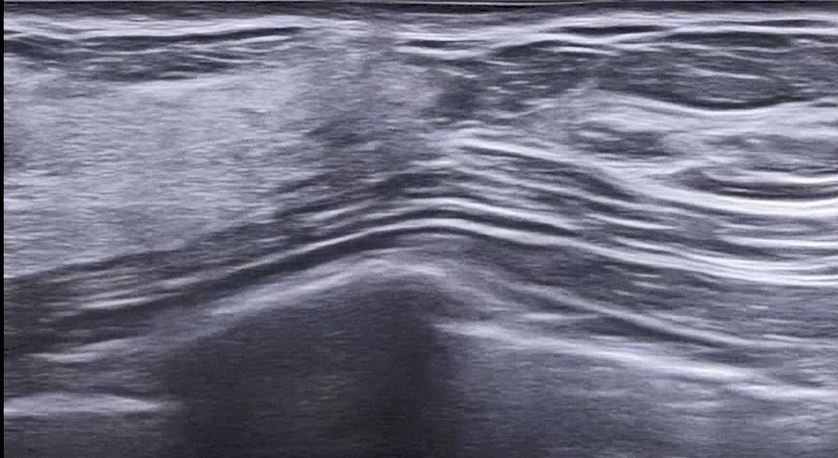
DVAE/EVAB or TVAE can be performed under ultrasound, X-ray or MRI guidance. The modality of choice is determined by the modality in which the lesion is best visualised and most readily accessible with the vacuum biopsy device7.
Performing a DVAE/EVAB – tips for success
- Review all baseline imaging–mammography/tomosynthesis/ultrasound and MRI if performed.
- Identify the abnormality for biopsy and if there is a marker clip already in place–is the marker clip adequately positioned?
- Adequate analgesia is important to ensure patient compliance during the biopsy. Normally 20 mL of 1% Xylocaine with adrenaline is used. It is important to create a cylinder of anaesthesia around the lesion to ensure the surrounding tissue is adequately anaesthetised, including tissue above and below the lesion.
- a. If performed Mammography- guided or MRI-guided, then this means giving analgesia in a clock face fashion at 12, 3, 6, and 9 o’clock. The anaesthesia also needs to extend from the skin to the lesion and beyond the lesion as the tip of the needle will be within normal breast tissue.
- b. If performed under US guidance, ensure that analgesia is given from the skin to the lesion and beyond the lesion. Use local anaesthesia medial, lateral, and inferior to the lesion. Ensure no gas is within the syringe and then administer a thin layer of anaesthesia above the lesion. This is important because on US the trough of the biopsy needle will lie beneath the lesion. The trough of the biopsy needle will be rotated, creating a semi-circle to ensure sampling the whole lesion. The superior aspect will include normal breast tissue and it is important that this is anaesthetised.
- Ensure the patient is in a comfortable position such that they can stay still for at least 20 minutes. Ensure, as the operator, you are in a comfortable position.
- Post-clip mammogram is important to assess clip position and to see if the original lesion is still visible or has been fully excised. Sometimes it is difficult to assess due to haematoma or post-biopsy changes and therefore the mammogram needs repeating 4-6 weeks later.

Photos used with the express permission of the author
VAE Complications
The most common complication is post-biopsy bleeding or haematoma. This can be minimised by appropriate compression of the area biopsied for 10 minutes, ensuring that the biopsy tract is not inadvertently being compressed, to ensure expression of the residual haematoma. If after 10 minutes bleeding persists, apply compression for another 10 minutes and finally apply a pressure bandage on the biopsy site.
Delay the post-clip mammogram if the patient bleeds beyond 10 minutes. Perform a few weeks later, ideally when the patient is coming back for follow up.
References
1 Marmot MG, Altman DG, Cameron DA, Dewar JA, Thompson SG, Wilcox M. The benefits and harms of breast cancer screening: an independent review. Br J Cancer. 2013 Jun;108(11):2205-40.
2 Morgan J, Potter S, Sharma N, et al. The SMALL trial: a big change for small breast cancers. Clin Oncol. 2019;31(9):659–663.
3 NHS Breast Screening Programme Clinical guidance for breast cancer screening assessment NHSBSP publication number 49 Fourth edition November 2016
4 Pinder SE, Shaaban A, Deb R, Desai A, Gandhi A, Lee AH, Pain S, Wilkinson L, Sharma N. NHS Breast Screening multidisciplinary working group guidelines for the diagnosis and management of breast lesions of uncertain malignant potential on core biopsy (B3 lesions). Clin Radiol. 2018 Aug;73(8):682-692.
5 Sharma N, Cornford E, Cheung S, Price H, Kearins O. The impact of vacuum-assisted excision in the management of indeterminate B3 lesions in the NHS Breast Screening Programme in England. Clin Radiol. 2021 Jun 1;76(6):470-e23.
6 McIntosh SA, Coles CE, Dodwell D, Elder K, Foster J, Gaunt C, Kirkham A, Lyburn I, Morgan J, Paramasivan S, Pinder SE. Abstract OT3-20-02: SMALL: Open Surgery versus Minimally invasive vacuum-Assisted excision for smaLL screen-detected breast cancer–a UK phase III randomised multi-centre trial. Cancer Research. 2023 Mar 1;83(5_Supplement):OT3-20.
7 Shaaban AM, Sharma N. Management of B3 lesions—practical issues. Current Breast Cancer Reports. 2019 Jun 15;11:83-8.
8 Yoo HS, Kang WS, Pyo JS, Yoon J. Efficacy and safety of vacuum-assisted excision for benign breast mass lesion: A meta-analysis. Medicina. 2021 Nov 17;57(11):1260.
9 Van De Voort E, Struik G, Klem T. Vacuum assisted excision as an alternative treatment option for benign breast lesions. Eur J Surg Oncol. 2021 Feb 1;47(2):e38-9.
10 Rageth CJ, O’Flynn EA, Pinker K, Kubik-Huch RA, Mundinger A, Decker T, Tausch C, Dammann F, Baltzer PA, Fallenberg EM, Foschini MP. Second International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast cancer Res Treat. 2019 Apr 15;174:279-96.
Guidelines+
European guidelines for the diagnosis, treatment and follow-up of B3 lesions
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European journal of heart failure. 2016;18(8):891-975. doi:https://doi.org/10.1002/ejhf.592
Pinder SE, Shaaban A, Deb R, Desai A, Gandhi A, Lee AHS, et al. NHS Breast Screening multidisciplinary working group guidelines for the diagnosis and management of breast lesions of uncertain malignant potential on core biopsy (B3 lesions). Clin Radiol. 2018 Aug;73(8):682-692.
Elfgen C, Leo C, Kubik-Huch RA, et al. Third International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Virchows Archiv: An International Journal of Pathology. 2023;483(1):5-20. doi:https://doi.org/10.1007/s00428-023-03566-x
Second International Consensus
Rageth CJ, O’Flynn EA, Pinker K, Kubik-Huch RA, Mundinger A, Decker, et al. Second International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat. 2019 Apr;174(2):279-296..
Rageth CJ, O’Flynn EA, Comstock C, Kurtz C, Kubik R, Madjar H, et al. First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat. 2016 Sep;159(2):203-13.
Clinical procedures+
US-guided VAB Clinical procedure 1
US- guided VAB Clinical Procedure 2
US- guided VAB Live Presentation

